“There’s a time and a place for antibiotics, you know. You don’t have to be a hero.”
I’d been struggling with a bad cold that turned into bronchitis and was rapidly moving into my lungs. It had been weeks of coughing up all manner of nastiness. I’d tried all my usual natural solutions, but nothing was working. I was depleted, exhausted, and just plain sick.
I was also stubborn, and well aware of the negative side effects of the gratuitous use of antibiotics. And I told her so.
“Margaret, this is no longer gratuitous.”
She had a point, and I gave in. I drove myself to urgent care, complaining the whole way, and sure enough, they prescribed antibiotics.
And they worked. Within days I was feeling significantly better. But I was too well informed to just be grateful. I knew the collateral damage I was doing to my gut and I was desperate to mitigate it.
This week, my fabulous colleague and friend Melanie Christner, NTP CGP, tackles this very subject.
How do you minimize the damage you do when you’re taking antibiotics?
Is it worth it to take probiotics at the same time, or should you wait?
If you do take the two at the same time, how do you get the most value from both?
These are great questions and Melanie has some great answers for you.
In an alternate universe…
…a cow’s growth spurt would be caused by a plump patch of alfalfa, NOT sub-therapeutic amounts of antibiotics.
…a child wouldn’t be given antibiotics for an ear infection. She would be treated quickly and effectively with natural alternatives.
…we wouldn’t be schooling naughty bacteria on how to avoid being ‘nuked’.
But, we live in this universe, and in this particular part of the universe, antibiotics have played the starring role in healthcare for too long. Their first minor role had the unglamorous title of “mould juice,” given by Alexander Fleming who first isolated the antibiotic penicillin from the fungus Penicillium. They quickly shot to stardom during WWII, upgraded to “The Wonder Drug.”
This lead role quickly bumped the other stars (those who played supporting roles like traditional food, herbs and homeopathic medicine), and like so many starlets, antibiotics got a little TOO popular, causing a tidal wave of reactions in the waterways, feedlots, and guts of the populace at large.
What’s really happening when you take antibiotics?
There are 9 main groups of antibiotics, grouped together based on how they work against certain bacteria.
These groups are:
- Penicillins – for example, phenoxymethylpenicillin, flucloxacillin, and amoxicillin.
- Cephalosporins – for example, cefaclor, cefadroxil, and cefalexin.
- Tetracyclines – for example, tetracycline, doxycycline, and lymecycline.
- Aminoglycosides – for example, gentamicin, and tobramycin.
- Macrolides – for example, erythromycin, azithromycin, and clarithromycin.
- Clindamycin.
- Sulfonamides and trimethoprim – for example, co-trimoxazole.
- Metronidazole and tinidazole.
- Quinolones – for example, ciprofloxacin, levofloxacin, and norfloxacin.
[Source]
How do they work?
It’s simple: antibiotics either mess with bacteria cell walls so that actively growing bacteria will burst and die, or they keep bacteria from multiplying by affecting their protein-building or DNA-copying machinery.
What’s the problem?
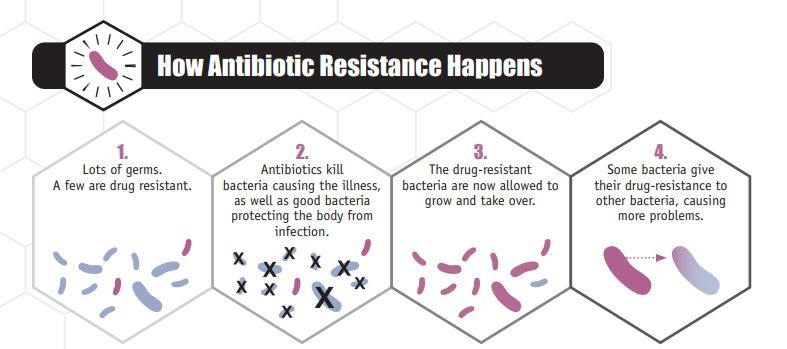
Antibiotics are indiscriminate.
To take the movie star analogy a little further…let’s say that antibiotics are called in to play a leading role in a car chase on some busy market street. There’s mayhem. Fruit carts overturned, people scrambling out of the way, property scraped up and damaged, metal flying…the movie focuses on the good guy chasing the bad guy, but not what is happening to the surrounding environment and people, who are devastated by the destruction.
That’s what it’s like when an antibiotic is administered to get rid of an infectious bacteria. The helpful bacteria are taken out along with the infectious bacteria. What does this do? It opens the way for the scavengers and pickpockets to take advantage of the confusion and set up shop, i.e. fungus and yeasts…which are NOT taken out by antibiotics. Some of the good guys never recover, and some take a really long time to recover. Antibiotic use also leads to antibiotic resistant strains of harmful bacteria, which we’ve aptly called “super bugs.”
[Source]
What the studies say
Just ONE course of antibiotics has the potential to permanently alter your gut microbiome. This study shows that one course of the antibiotic ciprofloxacin influenced about 1/3 of the abundance of bacteria in the gut. It took four weeks for most of the microbes to recover, however, several were still not recovered at six months.
This study and this one relate differences in babies born vaginally as compared to those born via C-section (whose mothers are given a prophylactic dose of antibiotics). The babies born via C-section have a different composition of gut bacteria than the babies born vaginally, and are more likely to have higher populations of C difficile bacteria. (As an aside, infants born full-term, vaginally at home, and were breastfed exclusively seemed to have the most “beneficial” gut microbiota – the highest numbers of bifidobacteria and lowest numbers of C difficile and E coli).
Infants born to women given antibiotics during pregnancy, or the 30% of children delivered via cesarean section, may be starting life with a significantly altered and insufficient level of friendly gut flora. This is a serious concern because lack of diversity in friendly gut bacteria has been shown to contribute to a large number of diseases and complications. ~Chris Kresser
This study shows that certain antibiotics disrupt mitochondrial activity in our cells, presumably because our mitochondria are very closely related to bacteria in their DNA.
Why is it important to keep our ‘good guys’?
Like a good neighbor…probiotics are there to take care of you and keep vigil in the neighborhood.
What are probiotics?
Here are some of the many ways probiotics help you out. Probiotics:
• determine whether some medications are toxic to your liver
• help digest your food (even taking genes from your food to help digest it!)
• may determine if your diet will work (i.e. weight loss attempts)
• train your immune system
• may influence your behavior (“My microbes made me do it!”)
• help you digest lactose — minimizing or eliminating lactose intolerance (NOTE: dairy that has been cultured at least 24 hrs. is lactose-free)
• help you digest protein — freeing the amino acids from protein
• balance your intestinal pH, lowering the colon pH
• improve or prevent irritable bowel syndrome
• halt and treat diarrhea from antibiotics, as well as prevent infection by producing antibiotic and anti-fungal substances.
• regulate peristalsis (movement of the bowel), improving bowel transit time
• reduce intestinal inflammation and protect your intestinal walls
• protect your gums and teeth
• make vitamins for you — B1, B2, B3, B5, B6, B12 & K
• make essential fatty acids and short-chain fatty acids (about 5-10% of them)
• convert flavonoids to usable forms
• increase absorption of minerals
• prevent food poisoning
• prevent and alleviate eczema, asthma, and allergies
• neutralize toxins, break down and prevent the production of bacterial toxins
• modulate autoimmune diseases
• support healthy blood pressure levels
• trigger hormones, as well as break them down and rebuild them
• promote optimal growth, healthy metabolism, and weight
• break down bile acids
• normalize serum cholesterol and triglycerides
• keep pathogenic yeasts (like candida) and pathogenic bacteria (like clostridium) in check and doing their assigned tasks
Wow. Probiotics are civic-minded champions!
What should I do if I, or my child, must take antibiotics?
We can minimize our need for antibiotics by feeding and nourishing our immune system with a traditional diet, moving our bodies regularly, and taking basic supplements. Learning natural alternatives and smart remedies for the occasions when someone is sick can also help you avoid the need for antibiotics. However, there are occasions in which you may not be able to avoid taking antibiotics, like strep throat, pneumonia, meningitis, etc.
Take probiotics concurrently (on the same days) as antibiotic treatment
If you must take antibiotics, the best course of action is to take probiotics concurrently (see below for effective strains and related brands). The studies show that specific probiotics taken at the same time as antibiotic medication both decrease the side effects and reduce the damage that antibiotics can cause in the gut microbiota. [Source]
Margaret’s note: I had minor surgery on my toe once when traveling in Italy. They prescribed antibiotics and when I went to the pharmacy to get them, they gave me the specific probiotic that would counter the damage done by the antibiotic along with it. I was very impressed, and I still wonder why we don’t do that here…
NOTE: DO take probiotics and antibiotics at different times of the day. A good rule of thumb is to leave two hours, or more, between taking antibiotics and probiotics.
Take the right strains (important!)
All of the strains listed below have been tested to be effective in mitigating or reducing the effects of antibiotics…but they are strain specific.
It is important to note that not all probiotic strains are created equal. All of the characteristics of good probiotics can vary, or not even exist, within the very same species of bacteria. The strain is what is listed after the genus (i.e. Lactobacillus) and species (i.e. rhamnosus).
All of the characteristics of good probiotics—able to withstand digestion, ability to stick to GI tract, able to multiply, and accurately identified—can vary, or not even exist, within the very same species of bacteria.
For example, Lactobacillus acidophilus DDS-1 is proven to survive the trek through the stomach acid and bile salts after ingestion, but many other Lactobacillus acidophilus strains will not survive even past the stomach. For another example, Lactobacillus rhamnosus GG is a strain that has studies to back up its effectiveness for a variety of conditions, like abdominal pain, antibiotic use, candida overgrowth, cystic fibrosis, dental caries, gastroenteritis and gestational diabetes.
4 options – probiotic strains that are effective with antibiotic use
OPTION #1 (single strain):
This strain is one of the most researched single strains. Thus it is the most easily accessible in a commercial sense. Best for finding quickly at your local pharmacy, and is good for avoiding or reducing traveler’s diarrhea. Does contain some fillers.
- Lactobacillus rhamnosus GG [Source]
Found in these brands:
- Culturelle (USA, UK, Canada)
- Metagenics (AU)
OPTION #2 (multiple strains):
This group of probiotic strains has been studied and found to be effective not only for diarrhea, but also for improving remission of ulcerative colitis, and reducing bloating and flatulence in IBS patients. Good for sourcing in the UK, as well as Australia, Canada, and the US.
- Bifidobacterium breve VSL,
- Bifidobacterium infantis VSL
- Bifidobacterium longum VSL
- Lactobacillus acidophilus VSL
- Lactobacillus delbrueckii ssp. bulgaricus VSL
- Lactobacillus paracasei VSL
- Lactobacillus plantarum VSL
- Streptococcus thermophilus VSL
[Source]
Found in these brands:
- Sigma Tau VSL#3 (USA)
- VSL #3 (UK)
OPTION 3 (single strain):
This strain is actually a beneficial yeast, rather than bacteria. It has the added benefit of being helpful for Clostridium difficile, some parasites, H. Pylori and can be part of an effective SIBO protocol.
- Saccharomyces cerevisiae variety boulardii (Biocodex strain) [Source]
Found in these brands:
- Biocodex Florastor (USA)
- Biocodex Florastor (Australia)
OPTION #4 (spore-based):
This is Margaret jumping in again to add in a fourth option I use all the time with my clients and family.
I love a spore-forming probiotic because, unlike other probiotics, rather than replacing individual strains, it works to adjust the overall terrain such that it favors the proliferation of the beneficial species, and discourages the proliferation of opportunistic bacteria. One of the reasons it can be so effective when used alongside antibiotics is that spores have a bi-phasic lifecycle that allows them to go dormant when under a stress such as antibiotics and then colonize in the large intestine when it’s safe due to quorum sensing (which is essentially how bacteria communicate with each other).
The product we use extensively and love is MegaSporeBiotic. One of the advantages of using extensive testing in my practice is that I see lots of “before” and “after” gut test results, and consistently I get the very best results with MegaSporeBiotic.
What should we do if I’ve already taken a course (or multiple courses) of antibiotics?
Don’t fret. If you’ve already taken one or more courses of antibiotics, it’s not too late to improve your digestive and whole body health. Here’s what I suggest:
- Heal the digestive tract. My favorite way to do this, because it’s almost entirely based on therapeutic foods, is the GAPS protocol. GAPS emphasizes removing difficult to digest foods, and eating healing foods like bone broth, healthy fats, and fermented foods on a regular basis.
- Introduce therapeutic amounts (see below) of beneficial probiotics for at least 6 months before moving to a maintenance dose. The maintenance dose is needed because you cannot “repopulate” the gut…you can only tip the balance by helping to keep a higher amount of helpful bacteria present in the gut.
Therapeutic doses
If you want to move the needle in your health with probiotics, you need to take enough, and for long enough. Once a therapeutic dose has been reached, it should be kept up for 6 months before reducing to a maintenance dose.
Remember to work up slowly to these doses, and when you start a new probiotic (with different strains) work up slowly again. Doses are in CFU’s, so if it says 1 – 2 billion per day, that means take whatever amount will give you 1 – 2 billion CFU’s per day.
I want to learn more about probiotics for my family, how can I?
I’m delighted you asked!
If you would like to:
- learn more about probiotics in general
- learn how to choose an effective one
- have an A – Z guide for conditions that are helped by specific strains
Then I invite you to check out my Mother’s Guide to Probiotics.

Melanie delights in helping you apply healing protocols to everyday life, while eating really great food…and becoming friends with your body again.
She writes at HonestBody.com. As a mom of four children herself, she works with moms and their kiddos to help them feel their best and to have all the life and energy they were meant to have.
Melanie is an NTP, Certified GAPS Practitioner, Restorative Wellness Practitioner, and Healing Foods Specialist in Vermont. Melanie’s passion is helping families navigate digestive therapy in a way that is understandable and well-supported. Having four children of her own, she loves working with children and families, and she endeavors to pair her desire to nourish with practical efficacy for clients.
Melanie works with clients one-to-one and leads families through her instructive and helpful GAPS Class, one class of several in the Honest Body Academy.
For fun you can either find her playing in her kitchen, or Nordic skiing, or swimming in the Green Mountain rivers with her family.




Try try ozone. We have other choices bronchitis well I use magnesium oil by Accent Minerals or cream from Elektra apply infar red heating pad to the chest area I like the one made from Battle Creek. Using anti Biotics is like saying how much gasoline can I ingest if I just dilute it. Although I’m aware when a cold esp in children takes a corner and you have another problem In hand but why not keep ACS silver nasal application or spray from Results RNA, magnesium topical application from ancient minerals or Elektra and the infar red heating pad in the emergency cabinet let’s teach ourselves better stronger methods that evoke health and long standing wellness.
Ah heck I used to keep a shovel in the shed to help with snow when it fell and an umbrella handy when it rained no difference here silver in the emergency cabinet magnesium beside the bathtub and the infar red handy for any muscle sprains or chest colds. Ozone and UVL at my favorite doctors office if it got out of hand
Just my 2 cents worth
Leslie Hamud, NTP
Leslie, I appreciate your comments. Trust me, in this case, I had tried ALL of it and I was progressing to pneumonia. There are times where it is actually appropriate to take antibiotics. But I agree with you completely – always reach for the natural remedies first and 9 times out of 10 you can get it. My immune system was absolutely fried in this case and it had been going on for near 6 weeks. It was time.
Thank you for this article. The only thing I would add is that one should never take the same probiotic long term. I took Bio-Kult for years while on GAPS and found out later I was wasting lots of money because my gut no longer benefitted from it who knows how long into taking it. Instead, one should change it up and try new brands/types every few months.
I was pleased to see this article and review/update my probiotic knowledge. I have been taking probiotics for almost a decade now. And they have made a HUGE difference in my overall health. If I do have to succumb to antibiotics (like now with an abcessed tooth) I take them in between doses of the antibiotic. I have been taking the same one for all this time (JarowDophilus 10 billion 8 strain). I have tried to vary it over the years, when I read articles like this. Every time i do, some of my old problems surface (skin rashes, mouth sores, vaginal yeast infections to name a few). So I don’t stray any more. But definitely I am better with them than without. I began taking them on the advice of an alternative health practitioner. Haven’t done anything to help my fibromyalgia, but I have a slew of other benefits. So they are worth the cost.
What about collodiol silver? Should children take it?
Hey, great post.
Fascinating to see that good bacteria are also taken out as well as bad bacteria.
Thanks for sharing the info about Probiotics